What is IBS?
Irritable Bowel Syndrome (IBS) is a common condition that impacts around one in five Australians at some point in their life, and is generally more common in women than men1. The exact cause of IBS is still unknown, but it is thought that genetics, age, diet and stress do play a role2.
There is currently no definitive cure for IBS, so it is recommended that people with IBS work with experienced practitioners to trial a combination of diet and other lifestyle changes to effectively manage their symptoms.
Do you think you may have IBS? Check in with your healthcare professional. Read more.
What are the different types of IBS?
There are four subtypes of IBS which are determined according to the main type of stool that is being passed3.
The types of IBS are classified as:
- IBS with constipation (IBS-C)
- IBS with diarrhea (IBS-D)
- IBS with mixed bowel habits (IBS-M)
- Unclassified IBS (IBS-U).
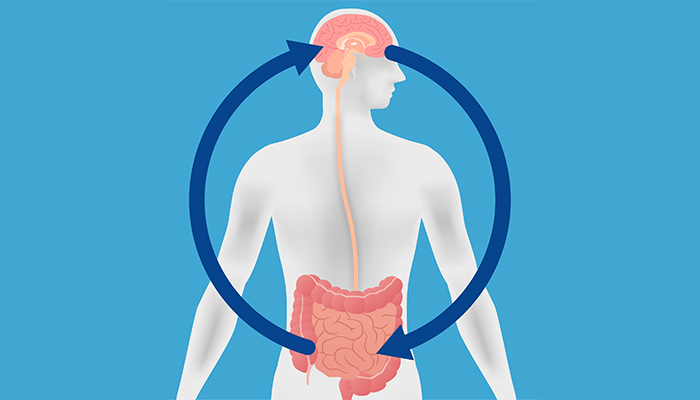
How is gut bacteria linked to IBS?
The gut microbiome is associated with many areas of health, including gut health. A growing body of research is aiming to understand how the gut microbiome differs in people who have IBS compared with those who do not.
What is currently known so far is that people with IBS have consistently been shown to have a lower diversity of gut bacteria than those people who do not have IBS4. The diversity of the microbiome refers to the balance of the bacteria, as it measures the total number of bacteria detected in the microbiome and compares how evenly they are spread. The microbiome in IBS also appears to be less stable and is quite susceptible to rapid changes5-6.
People with IBS have also been shown to have reduced levels of bacteria that produce beneficial Short Chain Fatty Acids (SCFAS), which help to lower inflammation and maintain good gut barrier function4. They also have increased levels of pro-inflammatory bacteria, some of which have been linked to a number of health conditions6.
These findings are also consistent with what Microba sees when analysing the data from our consented research participants.
What can you do if you think you may have IBS?
If you are concerned that you may have IBS, you should speak with a qualified healthcare professional as they are best placed to work with you on a diagnosis and treatment plan.
If you are interested in gut microbiome analysis and would like to speak with a health professional who is informed in the interpretation of the Insight™ report, please click here.
This microbiome test is not intended to be used to diagnose or treat medical conditions. A full disclaimer is available here
References
Kim, Y. S., & Kim, N. (2018). .
Sex-gender differences in irritable bowel syndrome. .
Journal of neurogastroenterology and motility, 24(4), 544.
Lovell, R.M., & Ford, A. C. (2012). .
Global prevalence of and risk factors for irritable bowel syndrome: a meta-analysis..
Clinical gastroenterology and hepatology, 10(7), 712-721.
Barbara, G., Grover, M., Bercik, P., Corsetti, M., Ghoshal, U. C., Ohman, L., & Rajilić-Stojanović, M. (2019). .
Rome Foundation working team report on post-infection irritable bowel syndrome. .
Gastroenterology, 156(1), 46-58.
Collins, S. M. (2014). .
A role for the gut microbiota in IBS. .
Nature reviews Gastroenterology & hepatology, 11(8), 497-505.
Chong, P. P., Chin, V. K., Looi, C. Y., Wong, W. F., Madhavan, P., & Yong, V. C. (2019). .
The Microbiome and Irritable Bowel Syndrome–A Review on the Pathophysiology, Current Research and Future Therapy. .
Frontiers in Microbiology, 10, 1136.
Salem, A. E., Singh, R., Ayoub, Y. K., Khairy, A. M., & Mullin, G. E. (2018). .
The gut microbiome and irritable bowel syndrome: state of art review. .
Arab Journal of Gastroenterology, 19(3), 136-141.