The truth about intermittent fasting and the gut microbiome
Author: Dr Kaylyn Tousignant
July 2021

Given its increasing popularity in recent years, you may have had patients asking you about intermittent fasting for weight loss, increased energy, and even mental clarity. So – when it comes to gut health, is intermittent fasting right for your patients?
An overview of intermittent fasting
The idea of intermittent fasting is to alternate between periods of eating and fasting, and there are several ways to do this. One popular method is the 16:8 protocol, where all meals are eaten within an 8-hour time window. Another approach is the 5:2 method, where calories are restricted for 2 days of the week and a regular, healthy diet is eaten for the other 5 days. Then there’s alternate-day fasting, which involves fasting (or calorie restriction) every other day. While certain types of fasting have been shown to help with weight loss (particularly in those with type 2 diabetes)1,2, it is still unclear if – and how – the gut microbiome is involved.
What does the science say?
Currently, most of the evidence we have for the effect of intermittent fasting on the gut microbiome comes from mice. The studies we do have in humans show some inconsistent results.
When looking at the 16:8 protocol, one study found that individuals who fasted had higher microbial richness compared to those who followed their usual eating patterns3. However, in a different study of the same fasting protocol, participants lost weight, but there was no impact on the gut microbiome4.
We have also gained important insights into the impact of fasting on the gut microbiome from individuals taking part in the Muslim holy month of Ramadan5-9, where no food is consumed from dawn to sunset. This model of religious fasting has been shown to have many health benefits, including weight loss, reduced cholesterol and improved blood sugar levels10.
Some studies have found that after Ramadan, individuals had increased levels of beneficial gut bacteria such as Akkermansia, Faecalibacterium and Roseburia5,6. They also had increased microbial richness and diversity and increased levels of the beneficial short-chain fatty acid, butyrate, which is generally associated with a healthy gut microbiome5,6,9. However, Ramadan affected different ethnic groups7 and age groups9 differently. This is a nice reminder that every patient has a unique microbiome, so while fasting might benefit some, it might not work for everyone.
Other types of fasting
So, what about different types of fasting? In a recent study using metagenomic sequencing, 71 individuals with metabolic syndrome were divided into two groups: both were put on a modified DASH (Dietary Approach to Stop Hypertension) diet for 3 months, but one group fasted for five days (300- 350 kcal/day derived from vegetable juice and vegetable broth) before beginning the diet11. Surprisingly, the fasting intervention led to weight loss and reduced blood pressure even 3 months post fasting, and this was not observed with the DASH diet alone.
Fasting induced substantial and significant changes in the microbiome and immune cells. While many of these initial shifts in microbiome composition reverted upon refeeding, levels of Escherichia coli and pro-inflammatory immune cells remained depleted. Interestingly, the levels of the butyrate-producing species, Faecalibacterium prausnitzii were not impacted by fasting but were shown to bloom during the refeeding period.
Some people responded better to the fasting and diet combination than others, with stronger improvements in blood pressure and reduced inflammation. Researchers could even predict who would benefit more from the intervention based on their starting gut microbiomes; ‘responders’ (i.e., those with a stronger reduction in blood pressure) initially had lower levels of bacteria that produce the short-chain fatty acid, propionate but these levels increased after fasting. By 3 months post fast, propionate production had reverted almost to baseline levels but the improvement in blood pressure remained, suggesting that transient improvement in propionate production stabilised a less hypertensive state by mechanisms beyond the gut.
This could explain why a systematic review of the effect of different types of fibre on blood pressure identified beta-glucan intake as having the strongest impact on blood pressure reduction13. As highlighted in the Insight™ microbiome report, beta-glucan is the prebiotic fibre of choice for improving microbial propionate production14.
So, what exactly is fasting doing to the microbiome?
Research in animal models is starting to give us clues into the ways that fasting affects the microbiome. These studies show several potential benefits, including increased microbial diversity, reduced inflammation, and increased production of short-chain fatty acids15,16. Intermittent fasting also decreased cognitive impairment and increased levels of tryptophan (a precursor for several hormones and neurotransmitters) and its metabolites 5-HT and IPA in the blood, suggesting a role of the gut-brain axis in mediating the effects of fasting15.
Time-restricted eating may also help regulate our circadian rhythm. Studies in mice and humans have shown that the composition and function of the microbiome fluctuates throughout the day, including changes in the production of SCFAs17-19. In mice, these SCFAs alter the expression of ‘circadian clock’ genes in the liver, which play an important role in the regulation of sleep, metabolism, and behaviour. While certain things can disrupt this rhythm (e.g., high-fat diets or jetlag), time-restricted feeding restored normal circadian patterns in mice and even prevented them from diet-induced weight gain17,18. This may be one way that fasting can influence your patient’s gut microbiome, however, more research in humans is required to tease apart this relationship.
Want to know which bacteria are associated with health & which are associated with disease? Find out in our Functions to Species Guide.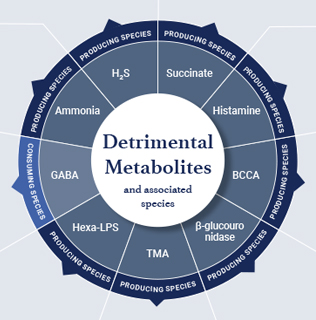
Is intermittent fasting right for your patients?
Despite compelling evidence in animal models, we still have a way to go to know how exactly intermittent fasting affects your patient’s gut microbiome, and in turn, their overall health. So far, the only metagenomic study exploring the impact of fasting in humans has highlighted the role of beneficial SCFAs, propionate and butyrate in blood pressure control. This raises concerns that fasting could have unintended consequences for health if it results in a reduction in dietary fibre intake. Even more, a popular starting point for intermittent fasting is to skip breakfast, but this could naturally cut out gut-healthy foods like whole grain oats, yoghurt, or fruit. No matter what time of the day, encouraging your patients to incorporate more plant-based, high-fibre foods into their diet is an important step towards improving their health.
The best way to know how a diet intervention is affecting your patient’s microbiome is to undertake a complete microbiome analysis using Insight™. Insight™ gut microbiome analysis can identify patients with a low number of species able to produce propionate which may identify them as ideal candidates for a fasting intervention or increased beta-glucan intake.
To discuss features of Insight™ including propionate and butyrate production, contact the healthcare team.
About the author

Dr Kaylyn Tousignant
References:
- Albosta, M. & Bakke, J. Intermittent fasting: is there a role in the treatment of diabetes? A review of the literature and guide for primary care physicians. Clin Diabetes Endocrinol, 2021;7, 3-3, https://doi.org/10.1186/s40842-020-00116-1.
- Borgundvaag, E., Mak, J. & Kramer, C. K. Metabolic Impact of Intermittent Fasting in Patients With Type 2 Diabetes Mellitus: A Systematic Review and Meta-analysis of Interventional Studies. The Journal of Clinical Endocrinology & Metabolism, 2020;106, 902-911. https://doi.org/10.1210/clinem/dgaa926.
- Zeb, F. et al. Effect of time-restricted feeding on metabolic risk and circadian rhythm associated with gut microbiome in healthy males. British Journal of Nutrition, 2020;2123, 1216- 1226. https://doi.org/10.1017/S0007114519003428.
- Gabel, K. et al. Effect of time restricted feeding on the gut microbiome in adults with obesity: A pilot study. Nutr Health, 2020;260106020910907. https://doi.org/10.1177/0260106020910907.
- Ozkul, C., Yalinay, M. & Karakan, T. Structural changes in gut microbiome after Ramadan fasting: a pilot study. Benef Microbes, 2020;11, 227-233. https://doi.org/10.3920/bm2019.0039.
- Özkul, C., Yalınay, M. & Karakan, Islamic fasting leads to an increased abundance of Akkermansia muciniphila and Bacteroides fragilis group: A preliminary study on intermittent fasting. Turk J Gastroenterol, 2019;30, 1030-1035. https://doi.org/10.5152/tjg.2019.19185.
- Ali, I. et al. Ramadan Fasting Leads to Shifts in Human Gut Microbiota Structured by Dietary Composition. Frontiers in Microbiology, 2021;12. https://doi.org/10.3389/fmicb.2021.642999.
- Mohammadzadeh, A. et al. The Interplay between fasting, gut microbiota, and lipid profile. International Journal of Clinical Practice, n/a;e14591. https://doi.org/10.1111/ijcp.14591.
- Su, J. et al. Remodeling of the gut microbiome during Ramadan-associated intermittent fasting. The American Journal of Clinical Nutrition, 2021;113, 1332-1342. https://doi.org/10.1093/ajcn/nqaa388.
- Trepanowski, J. F. & Bloomer, R. J. The impact of religious fasting on human health. Nutrition Journal, 2010;9, 57. https://doi.org/10.1186/1475-2891-9-57.
- Maifeld, A. et al. Fasting alters the gut microbiome reducing blood pressure and body weight in metabolic syndrome patients. Nature Communications, 2021;12, 1970. https://doi.org/10.1038/s41467-021-22097-0.
- Wang, D. D. et al. The gut microbiome modulates the protective association between a Mediterranean diet and cardiometabolic disease risk. Nat Med, 2021; 27, 333-343. https://doi.org/10.1038/s41591-020-01223-3.
- Evans CE, Greenwood DC, Threapleton DE, Cleghorn CL, Nykjaer C, Woodhead CE, Gale CP, Burley VJ. Effects of dietary fibre type on blood pressure: a systematic review and meta-analysis of randomized controlled trials of healthy individuals. J Hypertens, 2015 May;33(5):897-911. https://doi.org/10.1097/HJH.0000000000000515.
- Carlson JL, Erickson JM, Hess JM, Gould TJ, Slavin JL. Prebiotic Dietary Fiber and Gut Health: Comparing the in Vitro Fermentations of BetaGlucan, Inulin and Xylooligosaccharide. Nutrients, 2017 Dec 15;9(12):1361. https://doi.org/10.3390/nu9121361.
- Liu, Z. et al. Gut microbiota mediates intermittent-fasting alleviation of diabetes-induced cognitive impairment. Nature Communications, 2020;11, 855. https://doi.org/10.1038/s41467-020-14676-4.
- Zhang, X. et al. Effects of alternate-day fasting, time-restricted fasting and intermittent energy restriction DSS-induced on colitis and behavioral disorders. Redox Biol, 2020;32, 101535- 101535. https://doi.org/10.1016/j.redox.2020.101535.
- Leone, V. et al. Effects of Diurnal Variation of Gut Microbes and High-Fat Feeding on Host Circadian Clock Function and Metabolism. Cell Host & Microbe, 2015;17, 681-689. https://doi.org/10.1016/j.chom.2015.03.006.
- Zarrinpar, A., Chaix, A., Yooseph, S. & Panda, S. Diet and Feeding Pattern Affect the Diurnal Dynamics of the Gut Microbiome. Cell Metab, 2014;20, 1006-1017. https://doi.org/10.1016/j.cmet.2014.11.008.
- Kaczmarek, J. L., Musaad, S. M. & Holscher, H. D. Time of day and eating behaviors are associated with the composition and function of the human gastrointestinal microbiota. The American Journal of Clinical Nutrition, 2017;106, 1220-1231. https://doi.org/10.3945/ajcn.117.156380.