Stress and the gut microbiome
Author: Leanne Mitchell, Accredited Practising Dietitian, Microba Microbiome Coach
18 June 2020
Could stress be overtaking your patient’s gut health?
Navigating through the uncertainty of a pandemic truly makes us value our health. However, above and beyond the health impacts, this uncertainty brings with it a lot of stress which can impact our gut health!
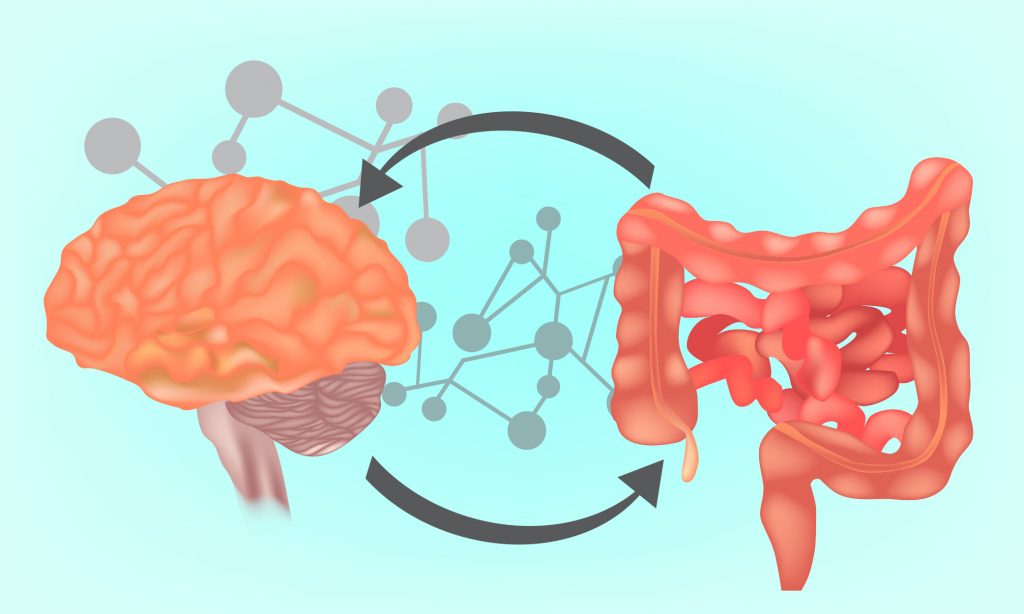
Brain to Gut: What happens to our gut when we are stressed?
When we are faced with a stressful situation our “fight or flight” mechanisms are activated. This sends a flood of stress hormones into our bodies. The main stress hormones are cortisol and adrenaline. With these hormones flying around the body, our heart rate and blood pressure increases, so too does our breathing and blood glucose levels. Interestingly, our digestive activity is also decreased or changed. For some, this can mean digestive processes stop, and for others it results in an urgent emptying of the bowels. Whichever the outcome, it is clear that stress affects digestive function.
But beyond functional changes, stress can also impact the composition and function of the gut microbiome – the community of microorganisms living in our gut. Animal studies have found that stress can make the gut and intestines more permeable, activating immune and pro-inflammatory responses which trigger additional stress hormones to be released1.
A recent study found that when healthy pregnant women were subjected to a social stress test, their changing cortisol levels were associated with shifts in the types and numbers of bacteria found in their gut2.
This may help explain why scientists have found that people with stress-associated conditions, such as depression and anxiety, have gut microbiomes that are different to healthy people3.
A 2018 review found that depressed people had increased levels of bacteria that are associated with poor health, such as those from the Proteobacteria phylum and the Eggerthella genus, while beneficial bacteria, such as those from the Prevotella, Ruminoccus and Coprococcus genera are decreased compared to healthy controls4.

Gut-to-brain: What does the research say? Find out from Biome-powered brain: a healthy gut could mean a healthy mind.
Gut to Brain: Can supporting our gut microbiome help manage our stress?
Our gut can communicate with our brain via multiple pathways including neural, hormonal, and immune. The main neural connection is through the vagus nerve5.
The vagus nerve runs the length of our body, connecting all our digestive organs, such as the stomach and intestines to our brain5.
This superhighway nerve allows the brain and gut to send signals to each other, however, most of the traffic runs in the direction from the gut to the brain5.
Serotonin, a neurotransmitter associated with mood and anxiety disorders, is one of the many substances that can activate the vagus nerve and send signals to the brain5,6.
Serotonin also plays a role in regulating our sleep, appetite and digestion and is, therefore, an important substance for our overall wellbeing7.
The majority of serotonin is produced in the gut by enterochromaffin (EC) cells which can be stimulated by the presence of the short chain fatty acids (SCFAs), butyrate and propionate6,7.
Want to know more about microbially produced serotonin? Read Serotonin: more than just a mood regulator.
SCFAs are anti-inflammatory substances produced by gut bacteria that feed on prebiotic fibres found in plant-based foods8,9.
One animal study found that mice treated with SCFAs were able to better tolerate stress, showing fewer signs of anxiety and depression than mice without this treatment10.
Of course, we are not mice but this research indicates the role diet may play in our ability to manage and respond to stress, a role which is mediated by our gut bacteria! Indeed, a recent study in healthy adults found that supplementation of the prebiotic fibre, β-galactooligosaccharides (B-GOS) was associated with a reduction in cortisol response upon waking11.
So, diets high in prebiotic, plant-based foods may help improve our overall sense of wellbeing and increase our stress tolerance.
Our gut bacteria are also able to produce GABA, another mood-associated neurotransmitter. Low brain (central) levels of GABA are often reported in people who suffer from depression12.
Animal studies have shown that the gut microbiome influences the circulation and brain levels of GABA13. However, in humans, it is unclear if the GABA produced by gut bacteria impact brain levels. Gut bacteria that produce GABA include species from the phyla, Bacteroides, Parabacteroides and Escherichia with a recent study finding that levels of Bacteroides were negatively correlated with brain patterns associated with depression14.
Many studies have shown a link between diet and the risk for depression15, and this could be in part due to the ability of diet to shape and alter the gut microbiome. A diet that continues to have increasing evidence showing benefits for depression is the Mediterranean diet16 which is a pattern of eating that is high in prebiotic, plant-based fibres.

Microba Senior Scientist, Dr Alena Pribyl explains the gut-brain axis in How smart is your is your gut? The gut-brain axis explained.
Practical strategies to help manage stress
You could assist your patients by recommending the following lifestyle interventions to help manage their stress, and in turn, support a healthy microbiome.
Gut to brain strategies: fuelling the microbiome through healthy eating.
- Recommend eating plenty of prebiotic, plant-based foods such as wholegrains, vegetables, legumes, nuts and seeds.
- Suggest your patient try going “Mediterranean”, or even meat-free, one to two days a week. They could enjoy large bowls of salad with legumes, roasted zucchini and quinoa stuffed capsicum or baked fish with roasted vegetables.
Brain to gut strategies: Supporting the microbiome through healthy activities.
- Exercise! Recommend your patient find an activity they enjoy or that they get on YouTube and follow along to a Zumba, circuit, or Pilates class. They could also make a home gym or go for a walk/run.
- Recommend your patient does something that brings them joy. This could include meditating, gardening, drawing, reading or simply soaking in the tub. The key is that they quiet the mind and find something that tunes out the world.
About the Author

Leanne Mitchell, APD
Leanne is an Accredited Practising Dietitian and works as one of the microbiome coaches at Microba. Leanne has a developing interest in the clinical application of the gut-brain axis in gastrointestinal disorders, mental health and neuro-developmental conditions.
References
- Dinan, T.G. and J.F. Cryan, Regulation of the stress response by the gut microbiota: Implications for psychoneuroendocrinology. Psychoneuroendocrinology, 2012. 37(9): p. 1369-1378.
- Hantsoo, L., et al., F160. Cortisol Response to Acute Stress is Associated With Differential Abundance of Taxa in Human Gut Microbiome. Biological Psychiatry, 2018. 83(9, Supplement): p. S300-S301.
- Anglin, R., et al., The Gut Microbiome in Patients with Anxiety, Depression and Inflammatory Bowel Disease. Neuropsychopharmacology, 2014. 39: p. S289-S289.
- Winter, G., R. Hart, and C. Sharpley, Gut microbiome and depression: what we know and what we need to know. Reviews in the Neurosciences, 2018. 29(6): p. 629-643.
- Breit, S., et al., Vagus Nerve as Modulator of the Brain–Gut Axis in Psychiatric and Inflammatory Disorders. Frontiers in Psychiatry, 2018. 9: p. 44.
- Mohajeri, M.H., et al., Relationship between the gut microbiome and brain function. Nutrition Reviews, 2018. 76(7): p. 481-496.
- O’Mahony, S.M., et al., Serotonin, tryptophan metabolism and the brain-gut-microbiome axis. Behavioural Brain Research, 2015. 277: p. 32-48.
- Koh, A., et al., From Dietary Fiber to Host Physiology: Short-Chain Fatty Acids as Key Bacterial Metabolites. Cell, 2016. 165(6): p. 1332-1345.
- Singh, R.K., et al., Influence of diet on the gut microbiome and implications for human health. J Transl Med, 2017. 15(1): p. 73.
- De Wouw, M., et al., Short‐chain fatty acids: microbial metabolites that alleviate stress‐induced brain–gut axis alterations. Journal of Physiology, 2018. 596(20): p. 4923-4944.
- Schmidt, K., et al., Prebiotic intake reduces the waking cortisol response and alters emotional bias in healthy volunteers. Psychopharmacology, 2015. 232(10): p. 1793-1801.
- Romeo, B., et al., Meta-analysis of central and peripheral γ-aminobutyric acid levels in patients with unipolar and bipolar depression. Journal of psychiatry & neuroscience : JPN, 2017. 43(1): p. 160228-160228.
- Strandwitz, P., Neurotransmitter modulation by the gut microbiota. Brain research, 2018. 1693(Pt B): p. 128-133.
- Strandwitz, P., et al., GABA-modulating bacteria of the human gut microbiota. Nature Microbiology, 2019. 4(3): p. 396-403.
- Lopresti, A.L., S.D. Hood, and P.D. Drummond, A review of lifestyle factors that contribute to important pathways associated with major depression: Diet, sleep and exercise. Journal of Affective Disorders, 2013. 148(1): p. 12-27.
- Sánchez-Villegas, A., et al., Mediterranean dietary pattern and depression: the PREDIMED randomized trial. BMC medicine, 2013. 11: p. 208-208.